After a dental implant procedure, there’s always a risk — no matter how small — that the implant may fail. However, a failed implant is different from an ailing implant. For an ailing implant, prompt treatment may be able to save the implant and prevent complete failure. However, leaving an ailing implant untreated can be detrimental and create a host of problems. An ailing implant is affected by peri-implant mucositis without bone loss. A variety of techniques can be used for surface decontamination, or a periodontist can choose to use a regenerative approach. A YAG laser, which is also used after cataract surgery to remove cloudiness of the artificial lens, can be used to effectively remove bacterial colonies and calculus from around the implant. While ailing implants were often hastily removed in the past, newer technology has allowed periodontists to help save implants from failure and it’s often not necessary to remove an implant affected by peri-implant mucositis right away.
Can Dental Implants Fail?
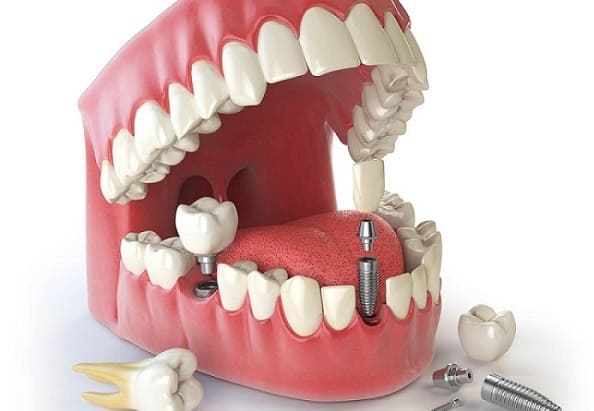
Dental implants are considered the “gold standard” in tooth replacement due to their reliability and long-term advantages to oral health and dental function. Though they have sustained over a 95 percent success rate, dental implants are unfortunately not immune to failure. The most common reason for failing dental implants is peri-implantitis, a condition characterized by infection and inflammation of the gum tissue surrounding implants. Similar in nature to gum disease, peri-implantitis has the potential to irreversibly damage the bone and soft tissue, ultimately leading to bone loss and failing dental implants. The beginning stages of this failure are often painless and may include tenderness or bleeding around the implant when brushed or minor bone loss that goes unnoticed by patients. If you have been experiencing similar symptoms, schedule an appointment with dentist.
Ailing and failing implant causes
Osseointegration Factors
Osseointegration is the process of the titanium implant fusing to your bone. It is often the case that the reason the implant is having issues is that certain protocols have not been strictly adhered to. The size and shape of the implants may have played a role. Length of integration times (premature loading) may play a role in conjunction with the type of bone that the implant was placed into, the types of bone grafting used in the guided bone regeneration procedures, and the overall oral and systemic health of the patient.
Mechanical Factors
Broken or fractured implant screws and abutments do occur and may play a role in this manifesting itself. If this does develop, the implant may require removal and the site need to be re-grafted. dentist will assess if a new implant is possible.
Fractured Implants
Defective implants do exist and can develop problems. Varied sizes and shapes of implants can become overburdened by the mechanical factors involved in chewing and once overloaded, implants can fail. If this is the case, the implant must be removed atraumatically so as to not extend the area of damage. Guided bone regeneration is generally also indicated.
Prosthetic Failures
The type of restoration and the type of materials used do play a role. From the materials used in fabricating single crowns and/or multi-unit restorations to the overall thought-process in carrying out a comprehensive restorative plan by the restorative expert—all of these factors must be well thought-out in maximizing the final result and avoiding potential pitfalls.
Implants can and do fail from time to time. Patients who suspect that they have an existing implant problem should seek an immediate evaluation from dentist before the problem progresses to include the surrounding teeth and bone.
Symptoms
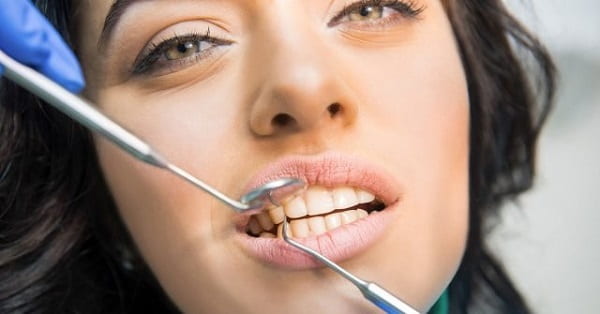
Gum Problems Are a Warning Sign
The first potential sign of trouble with dental implants is in the gums. The gums around your implant should be pink, healthy, and should stay at the same level on your implant. If your gums are red, inflamed, or are starting to recede around the dental implant, it’s time to be concerned. Fortunately, when we notice problems at this stage, we can typically reverse them and save the implant.
Most often, the treatment required at this stage is just a change in hygiene and maybe some antibiotics. The gums will recover, and can even regrow around the implant, especially if you have a metal-free implant, which is more compatible with both bones and gums.
Severe Gum Recession Means Bone Loss
If gum recession progresses further, and you have more exposed dental implant, then you’re experiencing bone loss around the implant. Some amount of bone loss is normal and may be expected, but it’s not a major concern. It does become a concern if the bone loss is exposing too much of the implant or is progressing too rapidly.
Bone is less likely to heal without intervention, so once you have bone loss, we’ll want to address it. One of the most common strategies is to do a bone graft similar to what was done when the implant was placed. Usually, though, the implant can stay in service, as long as it’s still firmly anchored in the bone.
A Loose Implant Is in Trouble
The most serious situation occurs when your implant is loose. Your implant should be firmly anchored in your jawbone and shouldn’t move. However, if your dental implant does move, it’s a sign that the implant may be failing. We might be able to stabilize it, but once the implant is loose we might have to remove it, heal the site, and replace it.
Targeted Treatment To Save Failing Dental Implants
The optimal treatment for implant failure depends on the underlying cause. Generally, your dentist or oral surgeon will need to remove the post and allow the area to heal. Your dentist can often treat peri-implantitis by cleaning the implant site and removing infected tissue. In cases where insufficient jawbone tissue led to implant failure, you will likely need a bone graft before your dentist can replace the post.
dentists use a revolutionary peri-implantitis laser technology to remove harmful bacteria and regenerate new tissue growth around ailing or failing dental implants. this protocol allows dentists to provide minimally invasive treatment that preserves the integrity of the soft tissue surrounding the implant, regenerates new bone and tissue growth, and accelerates healing times. Failing dental implants can also be treated using traditional dental tools that incise the gum tissue to gain access to the implant for detoxification and bone grafting, if necessary. While experiencing failing dental implants is a scary situation to be in, dentists have the experience and technology to accurately treat the problem, save your implant, and restore health to your smile.
Replacing a Compromised Restoration
While implant-supported restorations are more stable and secure than traditional options, they are not designed to last forever. They are subjected to daily wear and tear, which can affect their function. You may need to replace your restoration if you notice:
- Significant changes in the fit of the restoration
- Chips or fractures in the dental porcelain
- A loose restoration
- Excessive wear on the surface of the restoration
In most cases, implant-supported restoration can be replaced without surgery. Your dentist can fabricate a new crown, bridge, or denture and reattach it to the underlying abutment. If your restoration fails, contact your dentist immediately. Leaving a missing or damaged restoration untreated can cause more substantial oral health concerns.
How to prevent ailing and failing dental implant?
dental implants are, on the whole, very successful. Some clinical studies have shown 100% survival of implants up to 30 years, although most studies show survival rates of around 95% over 10 years.
But an important part of ensuring that your implants last 10, 20, or 30 years is taking proper care of them, watching for complications, and telling your dentist if anything does come up. It’s also important to have a dentist who is your long-term partner for ensuring the health, beauty, and function of your implants.
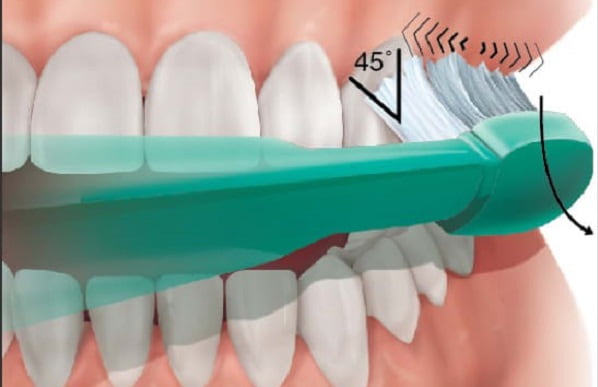
If issues surrounding your implant are identified early, your dentist may be able to save the implant without removing it. The best way to maintain the health of your dental implants is to practice good oral hygiene. Pay special attention to your implant-supported restoration while brushing and flossing. You should also attend regular cleanings and examinations at your dentist’s office about every three to six months. Your dentist can identify and treat any areas of concern as quickly as possible.